Epilepsy as a Whisper: Epidermoid Cyst Unveiled by Seizure Onset in Adolescence
DOI:
https://doi.org/10.3941/jrcr.5759Abstract
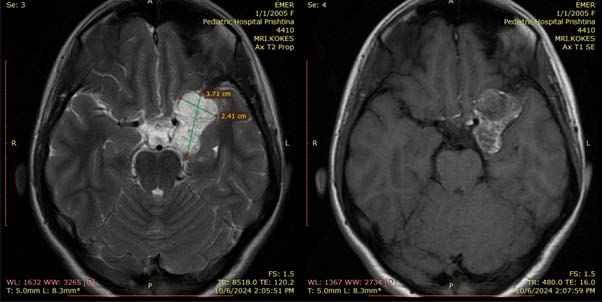
A 19-year-old female patient experienced her first epileptic seizure during a dental procedure, despite no prior history of seizures or epilepsy. Emergency imaging revealed a lobulated, well-circumscribed lesion located to the left frontotemporal basal region, measuring approximately 40×34×30 mm. MRI findings included hyperintense signal on FLAIR and DWI sequences, typical of epidermoid cysts, while CT revealed marginal calcifications without acute hemorrhage. The lesion exerted mild compression on adjacent structures, notably the left MCA and ICA, but showed no infiltration or edema. Diffusion-weighted imaging was critical in distinguishing the lesion from other cystic masses, demonstrating the classical diffusion restriction characteristic of epidermoid cysts. Epidermoid cysts are benign, congenital lesions accounting for only about 0.5–1.5% of all intracranial tumors, with common locations at the cerebellopontine angle and suprasellar cisterns; frontotemporal basal occurrence is exceedingly rare. Clinically, the patient reported longstanding intermittent headaches, nausea, vomiting, blurred vision, and later a second seizure while awaiting surgery. These symptoms, though nonspecific, underline the importance of considering epidermoid cysts in differential diagnosis when evaluating young patients with new-onset seizures and cystic lesions on imaging. Advanced imaging techniques such as DWI, FLAIR, and contrast-enhanced MRI were crucial in achieving a high preoperative suspicion for an epidermoid cyst. The lesion’s hypodensity on CT (measuring –15 HU) and hyperintense signal on T1W1-MRI in subarachnoid spaces suggested fatty contents, supporting the diagnosis of a perforated epidermoid cyst. Management was complicated by the lesion’s proximity to critical vascular structures, necessitating CT angiography prior to any intervention. Given the lack of local neurosurgical resources, the patient was referred abroad for advanced specialized treatment. External specialist reviews corroborated the imaging findings and recommended microsurgical resection with intraoperative neuro-navigation. Surgery was successfully performed in Turkey, with histopathology confirming the diagnosis of an epidermoid cyst. This case underscores the challenges posed by rare intracranial epidermoid cysts in both diagnosis and management, particularly when presenting in uncommon locations and healthcare settings with limited advanced surgical capabilities. It highlights the critical value of specific MRI sequences, especially DWI, in differentiating epidermoid cysts from other lesions such as arachnoid cysts or low-grade gliomas. Complete surgical resection remains the standard of care, although careful attention must be paid to preserving nearby vascular and neural structures to minimize postoperative deficits. Despite their benign nature, epidermoid cysts may recur if resection is incomplete, emphasizing the need for meticulous surgical planning and follow-up. The case also illustrates how epidermoid cysts, though congenital, often present clinically during adolescence or early adulthood, only after slow progressive growth leads to compression of adjacent structures. This case adds to the limited literature on intracranial epidermoid cysts involving the frontotemporal basal region and supports the recommendation for early differential diagnosis and the use of advanced imaging modalities to guide management decisions. Ultimately, it underscores the need for multidisciplinary coordination to achieve optimal outcomes for patients with complex, rare intracranial lesions.
Downloads
Published
Issue
Section
License
Copyright (c) 2025 Journal of Radiology Case Reports

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
The publisher holds the copyright to the published articles and contents. However, the articles in this journal are open-access articles distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 License, which permits reproduction and distribution, provided the original work is properly cited. The publisher and author have the right to use the text, images and other multimedia contents from the submitted work for further usage in affiliated programs. Commercial use and derivative works are not permitted, unless explicitly allowed by the publisher.