Subarachnoid and intraventricular dissemination of fat secondary to intrathecal pain pump
DOI:
https://doi.org/10.3941/jrcr.5676Abstract
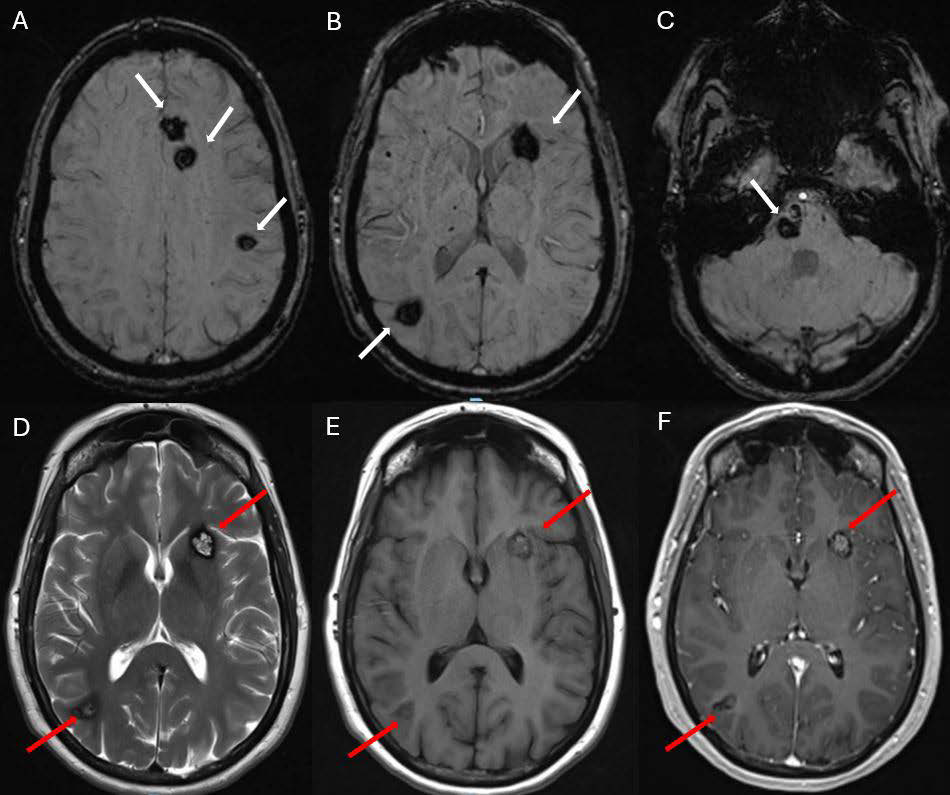
Radiologists frequently encounter intracranial fat in daily practice, typically representing physiologic or anatomic variations such as small fat deposits in the falx or well-known entities such as dermoid cysts, intracranial lipomas, and post-surgical/procedural dissemination after intracranial surgery and fat grafting. Among rare causes are subarachnoid and intraventricular migration of fat after spinal trauma or surgery.
A rarer entity, intracranial migration of fat following intrathecal pain pump placement, has been reported in only two previous cases in the English literature. With this article, we present the third documented case to raise awareness of this potential differential diagnosis for subarachnoid fat dissemination, particularly in the absence of a history of trauma or intracranial surgery. Given that the etiological source may be distant from the imaging field of view, it can easily be overlooked in the differential diagnosis.
Downloads
Published
Issue
Section
License
Copyright (c) 2025 Journal of Radiology Case Reports

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
The publisher holds the copyright to the published articles and contents. However, the articles in this journal are open-access articles distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 License, which permits reproduction and distribution, provided the original work is properly cited. The publisher and author have the right to use the text, images and other multimedia contents from the submitted work for further usage in affiliated programs. Commercial use and derivative works are not permitted, unless explicitly allowed by the publisher.